Total Joint Replacement Specialty Rating
Total joint replacement doctors for hip and knee pain
OrthoIndy total joint replacement surgeons specialize in replacing a joint damaged by trauma or arthritis with an artificial joint. It is now possible to replace most joints of the body. OrthoIndy total joint replacement surgeons focus on hip or knee replacement surgeries. However, some specialty physicians also do replacements on damaged joints other than the hip and knee.
When nonsurgical treatments have failed, joint replacement surgery may eliminate joint pain and restore range of motion.
Download Total Joint Replacement Guides
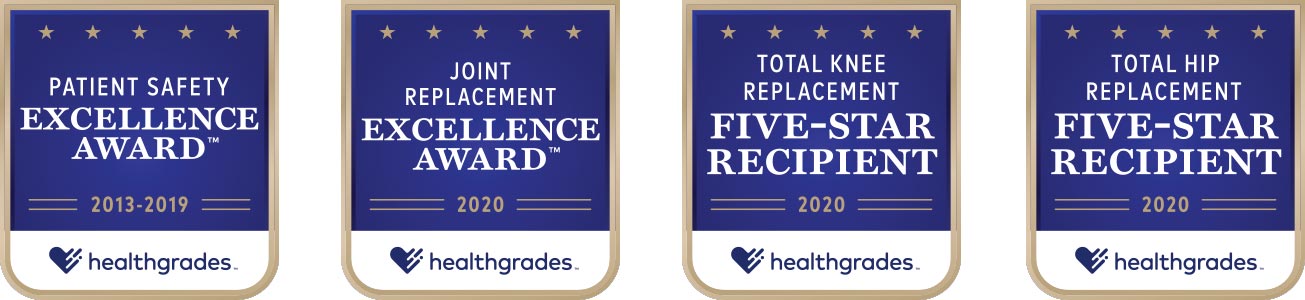
OrthoIndy Hospital has received numerous awards from Healthgrades for total joint replacement surgery.
Let's fix what hurts
Choose OrthoIndy to be your official orthopedic provider. We can help diagnose and treat any orthopedic injury or condition. The OrthoIndy total joint replacement specialists use the latest techniques to replace injured joints.
Meet the Team
Total Knee Replacement
The most common cause of chronic knee pain and disability is arthritis. Most knee pain is caused by one of three kinds of arthritis: osteoarthritis, rheumatoid arthritis or post-traumatic arthritis. Treatment includes:
- Total knee replacement surgery involves removing the diseased portion of the knee joint and resurfacing the ends of the bones with the new prosthesis.
- Physical therapy
Read The Ultimate Guide to Total Knee Replacement Surgery
Partial Knee Replacement
There are three compartments in a knee joint: a medial and lateral compartment between the ends of the femur (thigh) and tibia (shin) bones and the third compartment behind your kneecap. If only one of the compartments in your knee joint is affected by arthritis, it is possible that a total joint specialist can resurface in just that one compartment, leaving the other two healthy compartments alone. If that's the case, you may be a candidate for a partial knee replacement.
Learn More
Total Hip Replacement
The most common cause of chronic hip pain and disability is arthritis. Most hip pain is caused by one of three kinds of arthritis: osteoarthritis, rheumatoid arthritis or post-traumatic arthritis. Treatment includes:
- Total hip replacement surgery involves removing the diseased portion of the hip joint. An artificial hip, known as a prosthesis, replaces it.
- Physical therapy
rEAD THE ULTIMATE GUIDE TO TOTAL HIP REPLACEMeNT SURGERY
Signs it's time for a joint replacement
Hip and knee arthritis can be extremely uncomfortable and easily affect your quality of life.
If you are feeling depressed or frustrated because you can’t be as mobile as you want to be, these are signs you may need a total joint replacement and it’s time to speak to a total joint specialist about your options.
Signs you need a joint replacement include:
- Joint pain during activity
- Delayed joint pain after activity
- Pain that interrupts sleep
- Stiffness in your joint that makes it difficult to sit for long periods of time
- Inflammation and swelling in your joint
If you are experiencing any of the above symptoms, schedule an appointment with an OrthoIndy joint replacement surgeon.
Request an Appointment